Menu
Free Consultation
Dental implants have evolved dramatically over the last few decades. Today, endosteal (in‑bone) implants are the mainstream solution, but not everyone has enough jawbone volume to support them. For selected patients with severe ridge atrophy or those who wish to avoid major grafting, subperiosteal implants also called subperiosteal dental implants remain a purposeful alternative. This comprehensive guide explains what a subperiosteal implant is, who it’s for, how the process works from start to finish, and how it compares with other options, with practical FAQs like “a subperiosteal implant is commonly recommended for a …” and “do subperiosteal needs implant too?” (clarified below).
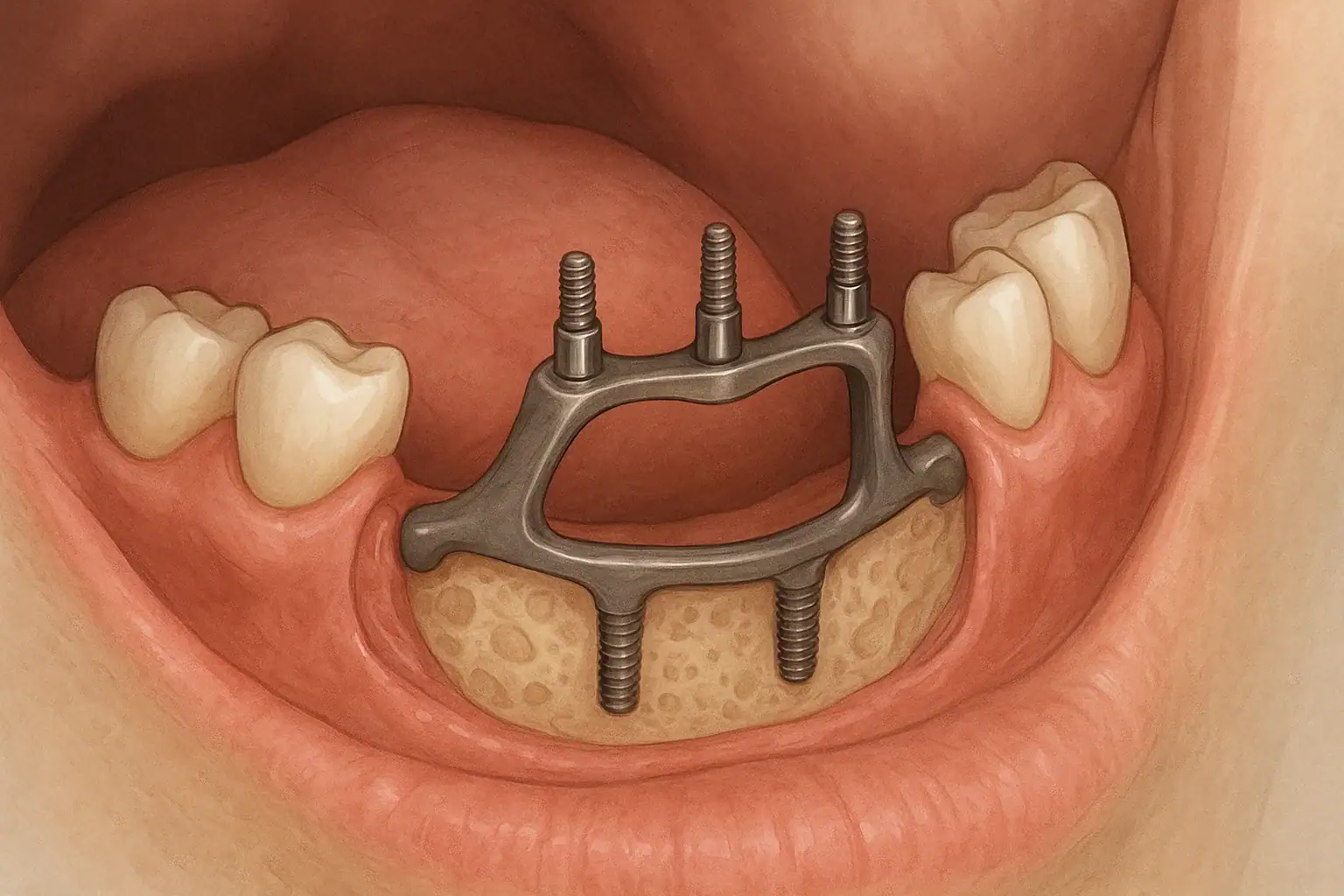
A subperiosteal implant is a custom-made metal framework (typically medical grade titanium) that sits on top of the jawbone but under the periosteum (the thin, vascular membrane covering bone). Transmucosal posts extend through the gum to support a fixed bridge or a removable overdenture. Unlike endosteal implants, subperiosteals do not rely on screw-shaped fixtures placed into the bone; instead, the framework is designed to rest over the bone surface and gain stability through intimate adaptation (and, in many modern designs, small fixation screws).
Key terms you’ll see used interchangeably:
A subperiosteal implant is commonly recommended for a patient who has one or more of the following:
Bottom line: Subperiosteal dental implants are case‑selective. An experienced surgeon will evaluate your bone anatomy, medical profile, and goals before recommending this path.
Modern CAD/CAM workflows transformed subperiosteals from analog frameworks into precisely fitted, patient‑specific devices.
| Solution | Best For | Main Trade‑offs |
|---|---|---|
| Endosteal Implants with Grafting | Patients who can tolerate bone augmentation and want in‑bone fixtures | More surgeries, longer timeline; widely available; high long‑term data |
| Zygomatic/Pterygoid Implants | Severe maxillary atrophy, especially posterior | Highly specialized; anatomical risks; generally avoids sinus grafting |
| Subperiosteal Implants | Severe ridge resorption with limited bone; graft‑averse or graft‑contraindicated | Soft‑tissue risk; fewer long‑term studies than endosteal; custom fabrication |
Materials: PMMA provisionals, then zirconia, hybrid titanium‑acrylic, or ceramic‑metal definitive prostheses depending on occlusion, esthetics, and budget.
Success depends on framework fit, tissue thickness, hygiene, occlusal balance, and provider experience. Well‑planned subperiosteals can deliver predictable multi‑year outcomes, particularly in full‑arch scenarios where alternative options are limited. As with any implant therapy, maintenance is the cornerstone of long‑term success.
Fees vary by arch, region, lab complexity, anesthesia, and provisional/final materials. While some policies offer partial coverage for surgical or prosthetic components, many cases are partly self‑pay. Request a written treatment plan that outlines surgical, prosthetic, maintenance, and potential revision costs.
Searching for “subperiosteal implants NJ”? When evaluating providers:
Helpful tip: Choose a clinic where the surgeon and prosthodontist plan your case together. Seamless surgical‑prosthetic coordination is vital for subperiosteal success.
Subperiosteal implants are custom titanium frameworks that sit on top of the jawbone, under the periosteum, with posts through the gum to support a bridge or overdenture. They are an option when bone is too thin/short for in‑bone (endosteal) implants or when patients want to avoid major grafting.
Same concept—the term refers to a subperiosteal dental implant framework that supports teeth without drilling long fixtures into bone.
It’s a patient‑specific metal framework designed from CBCT scans to rest over the jawbone and support teeth via transmucosal posts. Think of it as a custom “saddle” that shares chewing forces across a broad bone surface.
… patient with severe jawbone resorption, insufficient bone height/width for endosteal implants, failed or contraindicated grafting, or a desire to avoid extensive bone‑augmentation surgeries, especially in full‑arch rehabilitation.
If you mean “Do subperiosteal implants need bone grafts too?”—usually not. One of their key advantages is bypassing large grafts. Some cases may still benefit from minor soft‑tissue augmentation or small bone smoothing for better fit and hygiene access, but the major grafting often required for endosteal implants is typically avoided.
They are intended as a long‑term solution, but like any implant therapy, longevity depends on hygiene, bite forces, tissue health, and follow‑up care. Framework revisions are uncommon with good planning and maintenance.
Yes. Most full‑arch cases aim for a screw‑retained fixed bridge. Removable options (overdentures) can also be considered for hygiene or cost reasons.
Expect several days of swelling and a soft diet while tissues heal. Many patients transition from a provisional to a definitive bridge after soft‑tissue maturation and occlusal refinement.
They are safe in properly selected cases and when placed by experienced teams using modern CAD/CAM workflows, with strong emphasis on hygiene and maintenance.
Subperiosteal implants offer a viable, modern pathway for patients with severely resorbed jaws or for those wishing to avoid major bone grafting. With digital planning, custom titanium frameworks, and coordinated surgical‑prosthetic execution, they can restore chewing function, speech, and smile aesthetics when conventional endosteal implants aren’t an option.
If you’re exploring subperiosteal dental implants—whether locally or searching “subperiosteal implants NJ”—book a consultation with a team experienced in CAD/CAM subperiosteal frameworks. Request a comprehensive plan that includes diagnostics, timeline, materials, costs, and maintenance, so you know exactly what to expect.
